The ACOG had replaced the phrase 'Term pregnancy ' with 4 categories according to the weeks of pregnancy ( 37-42) as the fetal outcome differs from a category to another. These categories are:
Early term: from 37 weeks to 38 weeks, 6 days
Full term: from 39 weeks to 40 weeks, 6days
Late term: from 41 weeks to 41weeks, 6days
Post term : 42 weeks and more
( for detailed readings Medscape 22-10-2013)
Friday, November 1, 2013
Friday, June 7, 2013
Guidelines for endometrial assessment
A new clinical guide provides recommendations on endometrial assessment in perimenopausal and postmenopausal women and evaluates the indications and limitations of different assessment methods. The recommendations also address how to deal with inconclusive evaluations and persistent symptoms, as well as testing in women who use tamoxifen and unopposed estrogen.
Eva Dreisler, MD, from the Department of Gynaecology and Obstetrics at Copenhagen University Hospital Rigshospitalet in Copenhagen, Denmark, and colleagues from the European Menopause and Andropause Society report their recommendations in an article published online April 8 inMaturitas.
The recommendations are based on a review of the literature and a consensus of expert opinion. No single method is perfect, and a combination of methods may be necessary, the authors write.
"Speculum examination and palpation should always be done first to exclude non-endometrial gynaecological pathology," the authors write.
If speculum examination and cervical cytology have been assessed, transvaginal ultrasound scanning (TVS) should be performed initially because it is noninvasive and will measure endometrial thickness, as well as detect other pelvic pathology including leiomyomas and ovarian tumors. However, clinicians should be aware that the quality of ultrasound evaluation depends on the examiner's experience and the equipment used.
The primary indication for invasive methods should be to obtain endometrial tissue to diagnose or exclude endometrial cancer or premalignancies. Endometrial sampling can be done by dilatation and curettage or outpatient biopsy, using a disposable device. However, both procedures are "blind" and can miss focal lesions.
Hysteroscopy allows visually guided biopsies and the identification and removal of focal lesions, including endometrial polyps or submucous fibroids in the uterine cavity, but fibroids can obscure visualization. Previously, hospital admission and general anesthesia were required, but the procedure can now be performed in some cases in the office with local or no anesthesia.
"Diagnosing malignant and premalignant changes in the endometrium requires histology. However endometrial assessment is also required in various benign conditions such as investigation of abnormal uterine bleeding...and monitoring treatment of hyperplasia without atypia," the authors write.
Summary Recommendations
- Use TVS for initial assessment;
- perform endometrial biopsy as an outpatient procedure if possible;
- hysteroscopy provides direct visualization of the endometrial cavity and focal lesions;
- if results are inconclusive and abnormal uterine bleeding or postmenopausal bleeding continue, repeat TVS and perform hysteroscopy;
- endometrial thickness is increased in tamoxifen users, and hysteroscopy is recommended for postmenopausal bleeding in these patients;
- women who use unopposed estrogen therapy have an increased risk for endometrial cancer during and for several years after treatment is stopped, so continued assessment is recommended;
- endometrial assessment in the absence of bleeding should only be performed in women with high risk for endometrial cancer; and
- women who have no clear diagnosis or who have recurrent or persistent symptoms or previous hyperplasia should be followed-up, for example, after 6 months.
Brenda K. Jenkin, MD, a clinical professor of gynecology at the University of Wisconsin School of Medicine and Public Health in Madison, commented on the new guidelines in a telephone interview with Medscape Medical News.
"I have some hesitation about using ultrasound as the primary assessment tool in all age groups," Dr. Jenkin said. She was not involved in the development of the new recommendation.
"I recommend that practitioners follow the recent ACOG recommendations and use ultrasound as a tool to help in their assessment in certain situations, predominantly the postmenopausal patient," Dr. Jenkin explained.
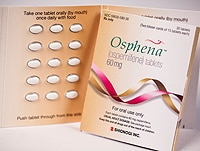
One coauthor reports speaking at national and international meetings for Novo-Nordisk, Schering Plough MSD, AstraZeneca A/S, Novartis and Sanofi Pasteur MSD, and advising Shionogi and Danish health authorities. One coauthor reports consulting for Bristol-Myers Squibb, Pfizer and AstraZeneca, primarily as an advisor on local legislations regarding medical information. Dr. Jenkin has disclosed no relevant financial relationships.
Saturday, May 25, 2013
Elective labor induction: still indicated?!
Elective Labor Induction May Soon Be Medical History
Kate Johnson
May 23, 2013
NEW ORLEANS, Louisiana — Policies restricting nonmedically indicated labor inductions are now in place in the majority of hospitals in the United States, and early signs are that they have the desired effect, according to several new studies.
"The national movement to eliminate non-medically indicated delivery at less than 39 weeks of gestation has prompted many hospitals to adopt specific policies against this practice," reported Nathaniel DeNicola, MD, from the University of Pennsylvania, in Philadelphia.
His survey, presented here at the American Congress of Obstetricians and Gynecologists (ACOG) 61st Annual Clinical Meeting, found that nearly two thirds of more than 2600 hospitals are on the bandwagon.
The majority, 67%, have a formal policy against nonmedically indicated labor induction, and among those without a formal policy, just over half said it was against their standard of care.
Dr. DeNicola found that 69% of formal hospital policies were hard-stop, meaning strictly enforced, as opposed to soft-stop or strongly discouraged.
"This represents a major step in promoting maternal and perinatal health," he said.
For Andrew Healy, MD, medical director of obstetrics at Baystate Medical Center, in Springfield, Massachusetts, the hard-stop policy has resulted in the expected, and even some unexpected, benefits.
"Something we didn't even anticipate as a benefit of this policy, but was a delightful surprise to see, was a decreased admission rate to the neonatal intensive care unit," Dr. Healy told Medscape Medical News at the meeting.
Angela Silber, MD, director of maternal-fetal medicine at Summa Akron City Hospital, in Ohio, said she found a similar decrease in neonatal intensive care unit (NICU) admissions after a hard-stop policy was implemented at her hospital. "You have less of the early term admissions for things that are not life-threatening, but still disruptive of the neonatal period that will affect breast-feeding and maternal-neonatal bonding," she said in an interview.
Both Dr. Silber and Dr. Healy presented studies at the meeting showing a range of benefits from their hospitals' new hard-stop policies.
"Before we had a policy against elective induction, but it wasn't being enforced," explained Dr. Healy. "We were seeing our c-section rate go up and patients on labor and delivery being induced for 2 and 3 days. We have also had an increase in the number of accreta cases, which is abnormal placentation in women who have typically had multiple c-sections; so, we're really trying to keep our c-section rate down."
Hard-Stop Policy Better Than Soft-Stop
Dr. Healy's study comparing 9515 singleton births before the policy and 2641 singletons after the policy found a significant decrease of 5.9 hours in the median time to delivery (P = .002).
The cesarean section rate for elective inductions also decreased from 16% before the policy to 7% after (P = .05).
NICU admission rates decreased by a third, he said. "Before the policy, 3% of term babies got admitted to the NICU and after the policy that went down to 2%" (P = .02).
"We didn't see any increase in the stillbirth rate, which is reassuring to all of us," Dr. Healy added.
Dr. Silber's similar pre- and postpolicy comparison also found a decrease in stillbirths and NICU admissions at her hospital.
Comparing 9806 singleton deliveries before the policy and 6041 singletons after, the number of stillbirths decreased significantly from 16 to 3 ( P = .023), with a trend toward significance in the reduction of NICU admissions (from 867 to 587; P = .06).
There was no significant difference in macrosomia rates (P = .718).
Other data from the study, which has not yet been fully compiled, shows a decrease in cesarean sections as well as postpartum hemorrhage, she added.
"Previously it was seen as not detrimental to a baby to be born at 37 or 38 weeks," she said, citing reasons such as patient discomfort, physician anxiety, and convenience as reasons for inductions.
Now, she says, her hospital may actually extend its hard-stop policy further to include patients beyond 39 weeks if they have an unfavorable cervix.
"And we're even considering stopping elective inductions completely — it's just a matter of time."
The researchers from all 3 studies have disclosed no relevant financial relationships.
American Congress of Obstetricians and Gynecologists (ACOG) 61st Annual Clinical Meeting: Abstracts 42 and 50. Presented May 6, 2013, and Abstract 44. Presented May 7, 2013.
Saturday, April 27, 2013
Red meat and egg yolk are risky
Intestinal Flora Again Implicated in CAD; but This Time, Also CV Events
CLEVELAND, OH — A major dietary source of choline provided in abundance by egg yolks and meat can, after conversion by intestinal bacteria, raise plasma levels of trimethylamine-N-oxide (TMAO), suggests a report published this week. It also supports earlier evidence that circulating TMAO is proatherogenic and may have potential as a biomarker of later cardiovascular risk.
The new study, actually a pair of prospective clinical studies, complement each other by establishing dietary phosphatidylcholine metabolism by gut flora as a source of circulating TMAO and TMAO levels as predictors of death, MI, and stroke "independent of traditional risk factors, even in low-risk cohorts," according to the authors, led by Dr WH Wilson Tang(Cleveland Clinic, OH).
Their work is detailed in the April 25, 2013 issue of the New England Journal of Medicine. If it sounds familiar, it may be because the same research team published strikingly similar findings two weeks ago in the journalNature Medicine , but naming dietary carnitine--also prevalent in red meat--as an ultimate source of TMAO released by intestinal microbiotia.
Our gut microbes are the biggest endocrine organ in our body. They can make biologically active compounds, and they contribute to disease processes.
The popular press seemed to enjoy itself in covering the study and exploded with stories, of varying accuracy, on how carnitine--also an additive to commercial energy drinks and diet supplements--may help drive the heart-disease risk associated with diets rich in meat.
(Later the same week, heartwire and others reported a meta-analysis suggesting, notably to a befuddled public, that L-carnitine given as a drug in acute MI could limit infarct size and improve clinical outcomes--proving as little else could that the overall story is more complicated than it seems.)
Dr Stanley L Hazen (Cleveland Clinic, OH), senior author of both reports linking food components to CV risk, told heartwire that it was an accident they appeared in the literature within two weeks of each other; with the manuscripts completed and submitted to different journals some time ago, they do not specifically cross-reference each other despite their close, complementary relationship.
More important, he said, their message isn't about L-carnitine or phosphatidylcholine. "It's all about the gut flora and TMAO, and TMAO is about cholesterol." The metabolite is thought to promote atherosclerosis, among other effects, "by changing cholesterol metabolism in the artery wall and other compartments like the liver and the intestines."
Taken further, the message is that "our gut microbes are the biggest endocrine organ in our body. They can make biologically active compounds, and they contribute to disease processes."
"A Truly Novel and Potentially Modifiable Risk Factor"
Hazen said the line of research began with observations by many in the field that the cardiovascular risk associated with diets rich in meat in epidemiologic studies far outstrips that expected from their cholesterol and saturated-fat content. So, the reasoning went, something else about meat seems to be adding to the increased risk.
The current study extends research in mice Hazen and his colleagues reported in 2011, which demonstrated a gut-flora–mediated relationship between dietary phosphatidylcholine, circulating levels of three metabolites (choline, TMAO, and betaine), and mechanisms behind arterial cholesterol buildup.
It to a large extent replicated those animal models clinically, with a focus on TMAO, in the test cohort of 40 healthy volunteers. Then TMAO emerged as an independent predictor of CV events in a separate cohort of >4000 patients undergoing elective angiography.
That the findings of the animal study also seem to apply to humans, Hazen said, suggests that TMAO might serve as a marker of CV risk and possibly a treatment target. And insofar that it points to a role for the metabolic effects of intestinal flora in atherogenesis, "it opens up new vistas for potential therapeutic approaches to go after for the treatment of heart disease."
In an accompanying editorial, Dr Joseph Loscalzo (Brigham and Women’s Hospital and Harvard Medical, Boston, MA) agreed, writing, "These studies in humans are consistent with the initial preclinical observations and point to a truly novel and potentially modifiable risk factor for atherothrombotic vascular disease."
"Unambiguous" Evidence
Forty healthy volunteers--no chronic illnesses (especially no heart, lung, or hematologic disease), no active infections, and no recent antibiotic therapy--were given a phosphatidylcholine challenge in which they consumed "two large hard-boiled eggs" and a capsule of deuterium-labeled phosphatidylcholine. Six of the participants repeated the challenge after a course of broad-spectrum antibiotics, which suppressed gut flora, and then again a month later after the gut flora had an opportunity to repopulate. Plasma and urinary choline metabolites, as products of ingested phosphatidylcholine, were measured after each challenge.
Measurement of deuterium levels by mass spectrometry showed that "a very large proportion" of urinary TMAO derived from the labeled ingested phosphatidylcholine, Hazen said. "It's unambiguous that phosphatidylcholine gets converted into TMAO." Moreover, urinary TMAO levels were closely correlated with plasma levels.
"Plasma levels of TMAO were markedly suppressed after the administration of antibiotics and then reappeared after withdrawal of antibiotics," the group writes. But postprandial plasma levels of the other two phosphatidylcholine products, free choline and betaine, were unaffected by antibiotic intake. That TMAO increased after the third phosphatidylcholine challenge pointed to resurgence of the intestinal flora.
Risk Doubled in "Low-Risk" Groups
The group also followed 4007 primarily male patients undergoing elective angiography for evaluation of possible coronary disease; none had experienced acute coronary syndromes. Those with baseline TMAO levels in the highest quartile, compared with the lowest quartile, showed an unadjusted hazard ratio (HR) for death, MI, or stroke of 2.54 (95% CI 1.96–3.28, p<0 .001="" after="" span="" three="" years.="">
The HR remained significantly increased at 1.88 (95% CI 1.44–2.44, p<0 .001="" 1.05="" 1.43="" ace="" adjustment="" after="" age="" and="" angiotensin-receptor="" aspirin="" beta-blockers.="" blockers="" blood="" body-mass="" c-reactive="" ci="" count="" diabetes="" filtration="" for="" further="" glomerular="" hdl-cholesterol="" index="" inhibitors="" it="" ldl-="" levels.="" levels="" myeloperoxidase="" of="" p="0.02)," pressure="" protein="" rate="" sex="" significant="" smoking="" span="" statins="" status="" still="" systolic="" total="" use="" was="" white-cell="">
Breaking the composite end point into components, the high-TMAO-level group showed an HR of 3.37 (95% CI 2.39–4.75, p<0 .001="" 1.48="" 2.13="" and="" ci="" death="" for="" mi="" nonfatal="" or="" p="" span="" stroke.="">
"Basically, none of the risk factors for atherosclerosis or CAD [we looked at] attenuated the intensity of this [TMAO] signal--it stays really robust." And, Hazen said, that applies to virtually all of the subgroups examined, including some that would traditionally be classified as lower risk. Those included those aged <65 a="" and="" baseline="" blood="" cad="" dl="" equivalents="" in="" ldl="" levels="" lipid="" managed="" markers="" mg="" nonsmokers="" normal="" of="" or="" other="" pressure="" primary-prevention="" setting.="" span="" those="" with="" without="">
"Even among subjects who were later categorized as not having significant CAD, because they had <50 a="" adjustments="" after="" and="" attack="" coronary="" death="" doubled="" even="" for="" hazen="" heart="" high="" it="" or="" risk="" said.="" significant="" span="" stenoses="" stroke="" their="" tmao="" was="">
In his editorial, Loscalzo writes that the current findings "raise the distinct possibility that atherothrombogenesis can be modulated or attenuated by a variety of novel strategies. These include, but are not limited to, modifying the diet to limit the intake of choline-rich food; altering gut microbiota with the use of probiotic approaches to limit synthesis of trimethylamine . . . or suppressing the synthesis of TMAO pharmacologically."
Supported by grants from the National Institutes of Health (NIH) and its Office of Dietary Supplements. The clinical study GeneBank was supported by grants from the NIH and a Cleveland Clinic/Case Western Reserve University Clinical and Translational Science Award. Hazen was supported by a gift from the Leonard Krieger Fund. Mass spectrometry instrumentation used was housed within the Cleveland Clinic Mass Spectrometry Facility with partial support through a Center of Innovation by AB Sciex. Tang reports consulting for Medtronic and St Jude Medical and receiving grants from Abbott Laboratories, St Jude Medical, Medtronic, and FoldRX. Hazen reports consulting for Abbott,Cleveland Heart Lab, Esperion, Lilly, Liposcience, Merck, and Pfizer and receiving grants from the NIH, Liposcience, Esperion, and the Leducq Fondation; and royalties from Abbott, Cleveland Heart Lab, Esperion, Frantz Biomarkers, Liposcience, and Siemens. Disclosures for the coauthors are listed at www.nejm.org.Loscalzo had no disclosures.
Anti-epileptic drugs
Antiepileptic drugs in pregnancy
It has long been believed that some antiepileptic drugs constitute a danger to the fetus. Generally women who suffer from epilepsy should stay on their medication during pregnancy because of the negative effects of seizures on mother and fetus. Certain agents are teratogenic but more subtle effects at lower doses may occur although they are less readily detectable. A new study by Meador et al (NEJM 2009;360:1597-605) is of considerable value in guiding prescribing.
The authors followed up the offspring of women taking single antiepileptic drugs (carbamazine, lamotrigine, phenytoin or valproate) at the age of 3 years and measured their neuro-developmental scores. Using IQ as the cognitive marker and after adjusting for maternal IQ, they found that the children exposed to valproate had scores 6 points lower than for carbazamine, 7 points lower than for phenytoin and 9 points lower than for lamotrigine. The association between valproate and IQ was dose dependant. This impairment of cognitive function should persuade women of childbearing age with epilepsy not to use valproate as their first-choice drug.
Saturday, April 20, 2013
Dyspareunia; surgery or low dose progestin both are effective
Dyspareunia: Surgery and Low-Dose Progestin Both Effective
Joe Barber Jr, PhD
Apr 17, 2013
Drug & Reference Information
Surgery and low-dose progestin are similarly effective against endometriosis-associated severe deep dyspareunia, but the timing of their effects differs, according to the findings of a patient-preference, parallel cohort study.
Paolo Vercellini, MD, from Università Statale di Milano and the Fondazione IRCCS 'Ca' Grandà–Ospedale Maggiore Policlinico in Milan, Italy, and colleagues present their findings in an articlepublished online February 26 and in the May issue of Human Reproduction.
"Painful sex also has personal and intimate implications, including substantial psychological and relational distress, as well as unfavourable emotional impact in partners," the authors write. "However, only limited information is available on the consequences of endometriosis-associated deep dyspareunia, as well as of the effect of medical and surgical treatment alternatives for this condition, in terms of variations in sexual functioning, psychological status and health-related quality of life."
Therefore, the authors recruited 18- to 40-year-old nonpregnant women who had previously undergone laparoscopy or laparotomy for stage 3/4 endometriosis in the previous 2 years and allowed them to select surgical or low-dose norethisterone acetate (NETA) treatment.
Among 51 women who underwent surgery and 103 women who selected NETA treatment, higher Female Sexual Function Index overall scores and subdomain scores were noted in the surgery group after 3 months, but the differences dissipated by 12 months, excluding the higher scores for lubrication, desire, and arousal in the surgery group.
However, significant differences from baseline were observed in the overall scores in both the surgery (P< .0001) and NETA (P = .002) groups.
The exclusion criteria included obstructive uropathy or bowel stenosis, typical contraindications to progestins, and an unwillingness to tolerate menstrual changes; the authors performed regression analysis adjusted for age, sex, body mass index, and other variables.
Similar to what was observed for Female Sexual Function Index scores, the Hospital Anxiety Depression Scale overall and subdomain scores were higher in the surgery group after 3 months, but these differences did not persist at 12 months. The overall and subdomain Hospital Anxiety Depression Scale scores were significantly lower after 12 months compared with baseline in both groups (P ≤ .0001).
For the Endometrial Health Profile-30 scores, the NETA group had significantly (P < .05) worse scores for the subdomains of pain, control and powerlessness, and medical profession. The surgery group had significantly higher Endometrial Health Profile-30 scores for the subdomains of emotional well-being, social support, self image, sexual intercourse, and infertility at 3 months, whereas significant differences in favor of the NETA group were observed for pain, control and powerlessness, relationship with children, work, and medical profession at 12 months.
The limitations of the study included a lack of randomization, selection bias, and an imbalance in the study groups.
"In conclusion, surgery and low-dose oral NETA demonstrated a similar final beneficial outcome in women with endometriosis-associated deep dyspareunia in terms of improvement of sexual functioning, psychological well-being and health-related quality of life at 1-year follow-up," the authors write. "[I]n light of the observed differences in the temporal pattern of the effect, further comparative studies with longer follow-up are warranted."
The study was supported by a research grant from the University of Milan School of Medicine. The authors have disclosed no relevant financial relationships.
Hum Reprod. 2013;28:1221-1230. Abstract
Wednesday, April 17, 2013
Ectopic Pregnancy Treatments Have Similar Fertility Impact
From Reuters Health Information CME
Ectopic Pregnancy Treatments Have Similar Fertility Impact
News Author: David Douglas
CME Author: Laurie Barclay, MD
CME Author: Laurie Barclay, MD
CME Released: 04/09/2013; Valid for credit through 04/09/2014

CLINICAL CONTEXT
To date, radical and conservative surgical treatments of ectopic pregnancy have not been compared in a randomized trial. Data were insufficient in a recent Cochrane review to draw conclusions regarding fertility after these treatments. However, fertility is similar after medical treatment and conservative surgery and is lower after radical surgery, based on prospective studies from ectopic pregnancy registries in 2 regions of France.
The objective of this study by Capmas and colleagues was to determine if treatment for the resolution of ectopic pregnancy affects subsequent spontaneous fertility with occurrence of an intrauterine pregnancy.
STUDY SYNOPSIS AND PERSPECTIVE
In women with ectopic pregnancy, both surgical and medical management have a comparable effect on later spontaneous fertility, according to French researchers reporting on the DEMETER trial.
"On one hand, for active ectopic pregnancy that requires surgical management, women can be reassured about their subsequent fertility even if a radical treatment is necessary as there is no difference between subsequent fertility after conservative or radical surgery," Dr. Perrine Capmas told Reuters Health by email.
"On the other hand," she added, "for less active pregnancy, women's preference is often medical treatment as there is no anesthesia and no surgery. However, as monitoring after medical treatment may sometimes be long, for some less observant women, conservative surgery should be offered as first-line."
In a March 12th online paper in Human Reproduction, Dr. Capmas of Hôpital Bicêtre, University Paris-Sud, and colleagues observe that improved diagnostic methods such as ultrasonography have made it possible to identify ectopic pregnancies earlier and more accurately, reducing serious adverse events.
Nevertheless, published data on fertility after various types of treatment is mainly observational. To gain further information, the researchers studied 406 women with ultrasound-confirmed ectopic pregnancy who were managed with either methotrexate injection to interrupt pregnancy in the Fallopian tube; conservative surgery (salpingostomy, which preserves the Fallopian tube); or radical surgery (salpingectomy).
The 207 women with a less active pregnancy (based on factors including Fernandez's score of less than 13 and no hemodynamic failure) were randomly assigned to receive conservative surgery followed by IM methotrexate or IM methotrexate alone.
In the remaining 199 women with active pregnancy, medical treatment was considered impractical because of clinical suspicion of rupture or a high Fernandez's score. These patients were randomized to conservative surgery followed by methotrexate or to radical surgery.
Two years later, rates of spontaneous intrauterine pregnancy in the less active pregnancy group were similar in those who had medical treatment, at 67%, and those who had conservative surgery, at 71%.
In the active pregnancy group, the rates were 70% after conservative surgery and 64% after radical surgery – again, not a significant difference.
Normal pregnancy rates in the general population in women who have not had an ectopic pregnancy range from about 84% to 89%.
Although the trial was conducted at 17 centers and sample sizes were small for some of them, the researchers say "the multicenter nature of the study provided a good external validity and, thus, a high level of evidence."
In particular, Dr. Capmas said in a statement, "If a woman has an active ectopic pregnancy for which surgery is the only treatment possible, then we can tell them that even if we try conservative surgery first, there is a risk they will need more radical surgery. However, we can tell them that subsequent fertility seems to be similar after each treatment."
Hum Reprod. Published online March 12, 2013.
STUDY HIGHLIGHTS
Subscribe to:
Posts (Atom)