
Friday, December 12, 2008
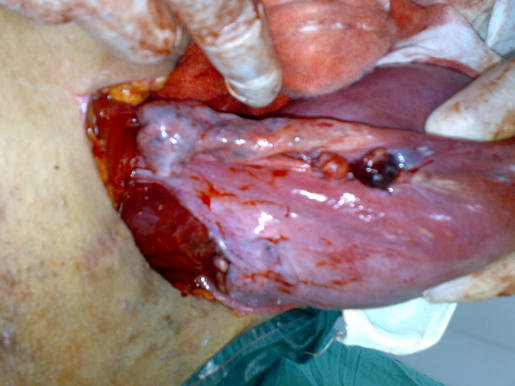
A CASE PRESENTATION - UTERINE SARCOMA

Sunday, November 9, 2008
Wednesday, May 28, 2008
GYNECOLOGICAL ANATOMY
PLEASE FOLLOW THE LINKS
http://www.mediafire.com/?sharekey=704223756825b0fcd2db6fb9a8902bda
- External genitalia
- FALLOPIAN TUBE
- PELVIC FASCIA
- PELVIC INNERVATION
- PELVIC LYMPHATICS
-PELVIC WALLS
- THE PERINEUM
- RECTUM AND ANAL CANAL
- THE SACRUM
- THE URETHRA
-THE VAGINA AND UTERUS
Monday, April 28, 2008
Tuesday, March 25, 2008
Sunday, March 23, 2008
GYNECOLOGY; FEMALE GENITAL INFECTION
http://www.salafishare.com/22MQV5NDRF8O/9QZLWPX.pdf
FOR PELVIC INFLAMATORY DISEASE (PID) FOLLOW THIS LINK
http://www.salafishare.com/2239Z667951S/I31VKC7.pdfl
FOR SEXUALLY TRANSMITTED DISEASES (STDs) FOLLOW THIS LINKS
http://www.mediafire.com/?tmbn3jzbmwb OR
http://www.mediafire.com/?tnkyiuxj93v OR
http://www.mediafire.com/?zyzpyyzfzsd
Friday, March 21, 2008
OPERATIVE OBSTETRICS; HUGE OVARIAN TUMOR WITH PREGNANCY
http://www.ups7.com/en/file/5743/heba-algazar-cs-20-3-2008--1--jpg.html
or this link

OPERATIVE GYNECOLOGY; CAH
http://www.ups7.com/en/file/5741/CAH2-jpg.html
http://www.ups7.com/en/file/5742/CAH--amputated-clitoris--jpg.html
or this link

OBSTETRICS; MULTIFETAL PREGNANCY
follow this link
http://www.ups7.com/en/file/5738/multiple-pregnancy-pdf.html
Multifetal pregnancy part two
follow this link
http://www.ups7.com/en/file/5740/multiple-pregnancy-2-pdf.html
Alternate links
http://www.mediafire.com/?c1indtnxnnj'>http://www.mediafire.com/?c1indtnxnnj
http://www.mediafire.com/?tdcgnm73rzm'">http://www.mediafire.com/?tdcgnm73rzm
ANATOMY OF THE FEMALE EXTERNAL GENTALIA
FOLLOW THE LINK
http://www.ups7.com/en/file/5735/ext--genitalia-pdf.html
other link
http://www.mediafire.com/?h1bqds55jimhttp://www.mediafire.com/?h1bqds55jim'>http://www.mediafire.com/?h1bqds55jim
Thursday, March 20, 2008
GYNECOLOGIC ONCOLOGY; OVARIAN CANCER
OVARIAN CANCER PART (1)
follow this link :
http://www.mediafire.com/?eixtlrmjxmp
OVARIAN CANCER PART (2)
link
http://www.mediafire.com/?x40zrr3yfx2
OVARIAN CANCER PART (3)
follow this link
http://www.mediafire.com/?dzxyd20mdzmhttp://www.mediafire.com/?dzxyd20mdzm'>http://www.mediafire.com/?dzxyd20mdzm
GYNECOLOGIC ONCOLOGY: GESTATIONAL TROPHOBLASTIC DISEASE (GTT)
GTT part (1) pdf
follow this link:
http://www.ups7.com/en/file/5708/GTT-1-pdf.html
other link
http://www.mediafire.com/?celmxzo4uaj
GTT part (2) pdf
follow this link :
http://www.ups7.com/en/file/5709/GTT-2-pdf.html
other link
http://www.mediafire.com/?zdtjkyxhtiihttp://www.mediafire.com/?zdtjkyxhtii'>http://www.mediafire.com/?zdtjkyxhtii
GYNECOLOGIC ONCOLOGY; ENDOMETRIAL CANCER
ENDOMETRIAL CANCER PART ONE follow the link
http://www.ups7.com/en/file/5901/endometrium-1-pdf.html
other link
http://www.mediafire.com/?wbjh0a9otwo
ENDOMETRIAL CANCER PART TWO follow the link
http://www.ups7.com/en/file/5706/endometrium-2-pdf.html
other link
http://www.mediafire.com/?nyjizv7j9je
Tuesday, March 18, 2008
GYNECOLOGIC ONCOLOGY; CANCER CERVIX (1)
folow this link:
http://up1.ups7.com/en/file/5615/cancer-cx-1-pdf.html
or this link
http://www.mediafire.com/?vesmkznj1ej">http://www.mediafire.com/?vesmkznj1ej'>http://www.mediafire.com/?vesmkznj1ej
NOTE that the Bethesda system was modified at 2001, the modification is as follows:
http://www.mediafire.com/?vesmkznj1ej
SPECIMEN TYPE: Indicate conventional smear (Pap smear) vs. liquid based vs. other
SPECIMEN ADEQUACY :
-Satisfactory for evaluation (describe presence or absence of endocervical/transformation zone component and any other quality indicators, e.g., partially obscuring blood, inflammation, etc.)
-Unsatisfactory for evaluation ... (specify reason)
- Specimen rejected/not processed (specify reason)
- Specimen processed and examined, but unsatisfactory for evaluation of epithelial abnormality because of (specify reason)
GENERAL CATEGORIZATION (optional)
- Negative for Intraepithelial Lesion or Malignancy
- Epithelial Cell Abnormality: See Interpretation/Result (specify ‘squamous’ or ‘glandular’ as appropriate)
- Other: See Interpretation/Result (e.g. endometrial cells in a woman ³ 40 years of age)
AUTOMATED REVIEW
- If case examined by automated device, specify device and result.
ANCILLARY TESTING
Provide a brief description of the test methods and report the result so that it is easily understood by the clinician.
INTERPRETATION/RESULT:
NEGATIVE FOR INTRAEPITHELIAL LESION OR MALIGNANCY (when there is no cellular evidence of neoplasia, state this in the General Categorization above and/or in the Interpretation/Result section of the report, whether or not there are organisms or other non-neoplastic findings)
ORGANISMS:
Trichomonas vaginalis
Fungal organisms morphologically consistent with Candida spp
Shift in flora suggestive of bacterial vaginosis
Bacteria morphologically consistent with Actinomyces spp.
Cellular changes consistent with Herpes simplex virus
OTHER NON NEOPLASTIC FINDINGS (Optional to report; list not inclusive):
Reactive cellular changes associated with :
-inflammation (includes typical repair)
-radiation
-intrauterine contraceptive device (IUD)
Glandular cells status post hysterectomy
Atrophy
OTHER
Endometrial cells (in a woman ³ 40 years of age)(Specify if ‘negative for squamous intraepithelial lesion’)
EPITHELIAL CELL ABNORMALITIES
SQUAMOUS CELL
Atypical squamous cells of undetermined significance (ASC-US)
cannot exclude HSIL (ASC-H)
Low grade squamous intraepithelial lesion (LSIL) encompassing: HPV/mild dysplasia/CIN 1
High grade squamous intraepithelial lesion (HSIL) encompassing: moderate and severe dysplasia, CIS/CIN 2 and CIN 3
with features suspicious for invasion (if invasion is suspected)
Squamous cell carcinoma
GLANDULAR CELL
Atypical
endocervical cells (NOS or specify in comments)
endometrial cells (NOS or specify in comments)
glandular cells (NOS or specify in comments)
Atypical
endocervical cells, favor neoplastic
glandular cells, favor neoplastic
Endocervical adenocarcinoma in situ
Adenocarcinoma
endocervical
endometrial
extrauterine
not otherwise specified (NOS)
OTHER MALIGNANT NEOPLASMS: (specify)
EDUCATIONAL NOTES AND SUGGESTIONS (optional)
Suggestions should be concise and consistent with clinical follow-up guidelines published by professional organizations (references to relevant publications may be included).
Saturday, March 15, 2008
VAGINAL VAULT PROLAPSE
pdf ( http://www.ups7.com/en/file/5703/Vault-Prolapse-pdf.html )
Wednesday, March 12, 2008
Anatomy of the vagina and uterus

ANATOMY : The pelvic colon, Rectum and Anus
follow this link
http://www.ups7.com/en/file/5717/rectum---anal-canal-pdf.html
ANATOMY OF THE PELVIC WALL
follow the ink
http://www.ups7.com/en/file/5728/pelvic-walls-pdf.html
other link
http://www.mediafire.com/?yhvyfc0wndk
ANATOMY OF THE PELVIC LYMPHATIC SYSTEM
follow the link
http://www.ups7.com/en/file/5732/pelvic-lYmphatics-pdf.html
other link
http://www.mediafire.com/?mdmv3yuu4xz
ANATOMY: PELVIC INNERVATION
follow the link
http://www.ups7.com/en/file/5734/pelvic-innervation-pdf.html
other link
http://www.mediafire.com/?iw8nvez0fwm
Anatomy of pelvic fascia
FOLLOW THE LINK
http://www.ups7.com/en/file/5736/pelvic-fascia-pdf.html
other link
http://www.mediafire.com/?3sygu75ndoc
Anatomy of the fallopian tube
FOLLOW THE LINK:
http://www.ups7.com/en/file/5737/fallopian-tube-pdf.html
other link
http://www.mediafire.com/?mx1xdyjua1w'>http://www.mediafire.com/?mx1xdyjua1w
Monday, March 3, 2008
OBSTETRICS; CARDIOVASCULAR DISEASES WITH PREGNANCY
Osama M. Warda, MD
follow the link for( pdf)
http://www.ups7.com/en/file/6155/CARDIOVASCULAR-DISEASE--students-pdf.html
anemia with pregnancy
By
Osama M. Warda, MD
follow the link (for pdf)
http://www.ups7.com/en/file/6154/ANEMIAS-DURING-PREGNANCY-pdf.html
Definition:
Anemia means reduction below normal of either red blood cells (RBCs) count, or hemoglobin percentage, or both leading to deficient oxygen carrying capacity of the blood.
During pregnancy; anemia is diagnosed if:
RBCs count is less than 3.5 millions/ cc OR,
Hemoglobin content less than 10 gm/dL , or
Hematocrit value is less than 30 %
Incidence:
- Anemia is the most common medical complication in pregnancy. More than 50% of all pregnant women in the USA (and much more numbers in the developing countries including Egypt) suffer anemia during pregnancy.
- Iron deficiency anemia is the most common type, followed by blood loss due to obstetric cause, and anemia due to chronic infection (see later under classification of anemia).
Anemia Pregnancy Inter-relations:
A]. Effect of anemia on pregnancy ( mother & fetus):
1- Increased incidence of Preeclampsia-eclampsia, especially with iron deficiency anemia and megaloblastic anemia (mechanism unknown).
2- Increased incidence of placental abruption (accidental hemorrhage).
3- Increased incidence of stillbirths, and neonatal deaths.
4- Increased incidence of preterm labor.
B]. Effect of pregnancy anemia:
Aggravation of the pre-existing anemia occurs due to;
1- Expansion of the maternal plasma volume (see physiologic changes due to pregnancy).
2- Fetal utilization of substrates necessary for building up of hemoglobin molecules.
Note Box ( )
Anemia of pregnancy (hyderemia; hemodilution):In pregnancy, a woman's blood volume increases by as much as 50 percent. This causes the concentration of red blood cells in her body to become diluted. This is sometimes called anemia of pregnancy and is not considered abnormal unless the levels fall too low.
Classification (types) of Anemia:
The simplest, yet effective, method of classifying anemia is according to the alteration of the blood indices, accordingly anemia may be hypochromic microcytic ( reduced indices), hyperchromic macrocytic ( increased indices), or normochromic normocytic ( un-altered indices).
[I]. HYPO-CHROMIC MICRO-CYTIC ANEMIA:
1- Iron deficiency anemia (most common).
2- Thalassemia (certain types).
3- Chronic infections (eg . glomerulonephritis, pyelonephritis).
4- Chronic lead poisoning.
5- Vitamin B6 deficiency.
[II].HYPER-CHROMIC MACRO-CYTIC ANEMIA:
1- Folic acid deficiency anemia.
2- Vitamin B12 deficiency anemia.
[III]. NORMOCHROMIC NORMOCYTIC ANEMIA:
1- Hemorrhagic anemia (due to blood loss).
2- Hemolytic anemias; (a) thalassemia, (b) sickle cell anemia, (c) spherocytosis, and (d) G6PD deficiency (= glucose-6-phosphate dehydrogenase deficiency)
3- Hypoplastic (aplastic) anemia.
IRON DEFICIENCY ANEMIA
It is the most common type of anemia encountered during pregnancy.
Physiological Role of iron during pregnancy:
Enters the haem portion of hemoglobin & myohemoglobin.
Respiratory enzymes as cytochrome oxidase enzyme.
Placental enzymes
Fetal hematopoeisis.
Metabolism of iron during pregnancy:
Normal diet supplies 14 mg of iron per day.
Only 1-2 mg ( 10-15% of dietary iron) is absorbed depending on iron stores (ferritin-apoferritin system).
Iron is absorbed in the 'ferrous' state in the presence of vitamin C. Phytate & phosphate decrease iron absorption .
Haem iron of red meat & liver is rapidly absorbed than vegetable iron in apple, spinache, and other vegetables.
Daily requirement of iron during pregnancy:
The daily requirement of the pregnant lady is 4 mg of elemental iron (it is 1mg for adult male, 2mg for the adult non-pregnant female).The total requirement during pregnancy is about 1000 mg of elemental iron calculated by the Council on Food and Nutrition as follows;
Þ To compensate for external iron loss…….= 170 mg
Þ To allow expansion of maternal cell……..= 450 mg
Þ Iron for fetal needs ………………………. =270 mg
Þ Iron in placenta and cord ………………….= 90 mg
Etiology of iron deficiency anemia during pregnancy:
[A]. Decrease intake of iron:
1. Poor diet.
2. Extensive morning sickness
[B]. Diminished absorption of iron:
1. Lack of vitamin C and proteins.
2. Increased phosphate & phytates.
3. Decreased gastric acidity & use of antacids.
4. Malabsorption syndromes, and parasitic infestations.
[C]. Increased iron demands during pregnancy:
1. Multiple pregnancy
2. Hemorrhage with pregnancy
3. Multi-parity
Clinical Picture:
S y m p t o m s:
1. General; pallor, tiredness, easy fatigability.
2. Cardiovascular; Dyspnea on exertion, palpitation, angina pains, swelling of lower limbs, and other low cardiac output symptoms.
3. Gastrointestinal; anorexia, nausea, vomiting, constipation.
4. Nervous System; lack of concentration, numbness and tingling, headaches.
S i g n s:
1. General; pallor, glassy tongue, brittle nails
2. Cardiovascular; haemic murmurs over the procordium on auscultation.
Investigations:
[A]. Peripheral blood ( complete blood count; CBC):
Findings suggestive of diagnosis include;
Microcytic hypochromic anemia ( ie, reduced indiced)
Anisocytosis (ie, different sizes of RBCs)
Piklocytosis (ie, different shapes of RBCs)
Normal reticulocytic count (ie, 0.5%- 1.5%)
Normal platelet & leukocyte counts
[B]. Blood chemistry:
Findings suggestive of diagnosis include;
Decreased serum iron less than 60µg/ dl (normal 90-150 µg / dl)
Decreased serum ferritin
Increased serum iron binding capacity more than 300 µg%
Increased free erythrocyte proto-porphyrin.
[C]. Bone marrow biopsy (seldom done):
There is absence of stainable iron in bone marrow.
Treatment of iron deficiency anemia during pregnancy:
[A]. Prophylactic Treatment:
Good pre-pregnancy nutrition not only helps prevent anemia, but also helps build other nutritional stores in the mother's body. Eating a healthy and balanced diet during pregnancy helps maintain the levels of iron and other important nutrients needed for the health of the mother and growing baby.
Every pregnant woman needs iron supplementation during pregnancy; the earlier the better ( but NOT earlier than 14 weeks pregnancy)
Oral iron supplementation to ALL pregnant ladies after 16 weeks gestation as 60-80 mg of elemental iron per day; can be obtained from;
Þ 200 mg ferrous fumarate, OR
Þ 300 mg ferrous sulfate, OR
Þ 550 mg ferrous gluconate, PLUS
Þ 1000mg vitamin C ( to help absorption) and 2mg folic acid (to help hematopoeisis). Antacids lower the absorption of iron from the stomach. [See appendix I ]
[B]. Active Treatment:
Active management of anemia depends on 2 main factors; severity of anemia, and the duration of pregnancy.
(1). Pregnancy 16-30 weeks: Oral ferrous sulfate 300mg t.d.s (ie, 900mg per day, or triple the prophylactic dose). This treatment is supposed to increase the hemoglobin concentration by 1 gm per month.
(2). Pregnancy after 30 weeks with severe anemia: parenteral iron therapy is indicated. Iron preparation can be given via intramuscular injection (eg, iron sorbitol; imferon®: 250mg every other day) or intravenous infusion in a crystalloid solution (eg ferrous succinate; ferosac®: 1amp in 100 ml of dextrose 5% every other day). [See appendix II]
Side –effects of iron therapy:
- Oral iron preparations may cause gastric upsets, constipation, dark green or black stools
- Parenteral iron preparations may cause pain & staining at the site of injection, hemosiderosis, and also anaphylaxis.
(3). Anemia after 35 weeks pregnancy and hemoglobin less than 6 gm/dl:
These patients should receive transfusion of packed RBCs (or whole blood if packed RBCs are not available). However, transfusions carry the hazards of transmission of viral infection, and transfusion reactions.
Folic Acid Deficiency Anemia
Folic acid deficiency causes megaloblastic anemia which is uncommon type of anemia during pregnancy accounts for 3% of cases of anemia during pregnancy.
Folic acid metabolism during pregnancy:
Pregnancy is associated with negative folate balance.
Folic acid & iron play a central role in nutrition & DNA synthesis.
Folic acid is reduced by reductase enzyme, giving dihydrofolic acid, which is further reduced by the same enzyme giving tetrahydrofolic acid (ie, folinic acid).
Folinic acid is necessary for DNA synthesis, cell growth, cell division, epithelial cells, and bone marrow cells.
Folate requirements are increased during pregnancy for the growing fetus, placenta, maternal RBCs, and uterine hypertrophy. Folate requirement in normal pregnant lady are 200-300 µg/ day.
Etiology of folic acid deficiency anemia:
The causes are the same as those of iron deficiency anemia (see before), plus the following:
Anti-convulsion therapy (eg, pregnant epileptic patient on epanutin®).
Antipyretic therapy.
Chronic hemolysis.
Investigations for folate deficiency:
[A]. Peripheral blood:
The findings suggestive of diagnosis:
· Macrocytic hyperchromic anemia (MCV increased)
· Hypersegmented polymorphs
· Elevated reticulocytic count.
[B]. Blood chemistry:
Decreased plasma folate level; the finding of a serum folate <2ng/> 2%)
Elevated indirect serum bilirubin.
Shortened life span of RBCs (by isotope chromium 51).
Erythroid hyperplasia of the bone marrow.
Hemoglobinopathies
Introduction:
Hemoglobin molecule is formed of 2 parts; haem which is an iron containing porphyrin, and globin which is a protein formed of 2 pairs of polypeptide chains (in the adult hemoglobin they are 2 α chains and 2β chains). Genes responsible for α chains are carried on chromosome 16, while those responsible for β chains on chromosome 11.Abnormalities in synthesis of either chain is genetically determined and result in thalassemia which are causes of anemia. On the other hand, in sickle-cell hemoglobinopathies, the polypeptide chains of hemoglobin are normal except for the amino acid sequence which is abnormal with replacement of glutamic acid by valine at the 6th position leading to formation of hemoglobin- S which is abnormal.
Thalassemias:
§ There are 2 main forms of thalassemia namely; the α- thalassemia due to inadequate synthesis of the α-chains, and the β- thalassemia due to inadequate synthesis of the β-chains.
§ Thalassemias are genitically determined & inherited as autosomal recessive.
§ Thalassemias are found throughout the world but centered in the Mediterranean are, Middle East, South-east Asia, and in India.
§ The clinical varieties of α- thalassemia are variable from lethal form (not compatible with extra-uterine life and causes hydropes fetalis to the affected fetus), to sub-clinical carrier types. The milder forms can be encountered in the pregnant lady with anemia.
§ Beta –thalassemias are either major (when the deficiency of the β-chain is homozygos), or minor (when the deficiency of the β-chain is heteozygos). Only the minor types can be encountered in the pregnant woman.
Management of pregnancies complicated by thalassemias:
[A]. MATERNAL: (with the aid of a hematologist)
No specific therapy for β-thalassemia minor during pregnancy; as the outcome for both the mother & the fetus is satisfactory.
Blood transfusion is rarely indicated except for hemorrhage.
Prophylactic folic acid supplementation is strongly indicated.
Proper treatment of infections.
Iron chelating agents (eg, Desferal®) are indicated.
[B]. FETAL:
The fetal management in patients with thalassemia or sickle cell disease is concerned with the fetal risk of acquiring the disease. Management consists of:
Genetic counseling to determine the fetal risks by Mendelian laws.
Antenatal diagnosis of thalassemias & sickle cell anemia may be achieve via one of the following techniques:
(a) Chorionic villus sampling,
(b) Early amniocentesis between 7-11 weeks gestation,
(c) Cordocentesis through percutaneous umbilical blood sampling (PCUBS), or
(d) Fetoscopy with cord blood sampling.
3. Termination of pregnancy is considered if the fetus is severely affected.
4. Reassurance of pregnancies if the fetus is not affected or mildly affected.
Sickle-cell Hemoglobinopathies:
Again the abnormality here is the replacement of the glutamic acid by valine at the position 6 on the polypeptide chain of hemoglobin leading to formation of hemoglobin-S.
Sickle-cell disease is inherited as autosomal recessive ( as thalassemia).
There are 4 types; sickle cell anemia (SS-disease), sickle-cell trait (SA-disease), sickle cell- hemoglobin C disease (SC-disease), and sickle cell - β-thalassemia disease (SB-disease). All (except the first type) are mild forms with no significant maternal complications.
Sickle-cell anemia (SS-disease) and pregnancy:
Incidence:
Sickle –cell anemia is common among black races. The theoretical incidence during pregnancy is 1:600 pregnancies. However it seems to be not so common due to high death rates among children with the disease, and lower parity of women with the SS- disease.This disease is almost unknown among Egyptian pregnant women.
Effect of sickle cell anemia on pregnancy, delivery, and puerperium:
It has a very bad outcome for both the mother and the fetus
[A]. MATERNAL:
Maternal mortality is 6% due to the following complications:
1. Severe anemia.
2. Sickle cell crisis; including hemolytic crisis, sequestration crisis, aplastic crisis, and thrombotic crisis.
3. Infections; pulmonary infections with pneumonia, chest infections, and urinary tract infections.
[B]. FETAL:
Bad as about 50% of pregnancies end by abortion, stillbirth, low birth weight infants, or neonatal deaths.
Management of pregnancies complicated by the SS-disease:
[A]. PREGNANCY:
Very close observation (frequent antenatal visits, or hospital admissions).
Folic acid supplementation ( 2mg orally / day).
Eradication of asymptomatic bacteruria & pyelonephritis.
Guard against pneumonia and heart failure.
Prophylactic blood transfusion.
Management of crisis by:
a) Oxygenation
b) Hydration (iv fluid therapy)
c) Blood transfusion
d) Heparinization for the thrombotic cricis
[B]. DELIVERY: (managed as cardiac patients)
Comfortable but not sedated.
Blood ready for transfusion.
Vaginal delivery is preferred, and CS for obstetrical indication only.
Regional anesthesia is better than general anesthesia.
Replace blood loss adequately.
[C]. CONTRACEPTION:
Tubal sterilization is indicated even if the parity is very low.
Combined oral contraceptives are contraindicated (↑thrombosis)
Intrauterine contraceptive device (IUCD) is contraindicated (↑infection).
APPENDIX ( I ):
Iron-containing foods:
Good food sources of iron include the following:
meats - beef, lamb, liver, and other organ meats
poultry - chicken, duck, turkey, liver (especially dark meat)
fish - shellfish, including clams, mussels, oysters, sardines, and anchovies
leafy greens of the cabbage family, such as broccoli, kale, turnip greens, and collards
legumes, such as lima beans and green peas; dry beans and peas, such as pinto beans, black-eyed peas, and canned baked beans
yeast-leavened whole-wheat bread and rolls
iron-enriched white bread, pasta, rice, and cereals
Monday, January 21, 2008
MOLAR PREGNANCY
http://www.salafishare.com/22NR50KLBPQG/LMJX85H.doc
Definition
Incidence
Clinical course
Diagnosis
Prognosis
Treatment
__________________________________________________________________
Definition
It is an abnormal pregnancy characterized clinically by abnormalities of the chorionic villi, consisting of varying degrees of trophoblastic proliferation & edema of the villous stroma.
Site: moles usually occupy the uterine cavity; however it may occasionally located in the fallopian tube or even the ovary.
Types:
According to presence or absence of a fetus, or embryo; it may be partial or complete mole.
Differences between complete and partial molar pregnancy:
PARTIAL MOLE MOLE
[A]. Karyotype :69 xxx, or 69 xxy(triploidy)
[B]. Pathology:
1- fetus: Present
2- amnion, fetal RBCs: Present
3- villous edema: Variable, focal
4- trophoblast proliferation: Focal , moderate
[C]. Clinical presentation
1- diagnosis: Missed abortion
2- uterine size: Small for date
3- theca lutein cysts**: Rare
4- medical complications: Rare
5- postmolar disease: 5-10%
COMPLETE MOLE
[A]. Karyotype: 46xx or 46 xy(paternal: androgenesis)*
[B]. Pathology:
1- fetus: Absent
2- amnion, fetal RBCs: absent
3- villous edema : diffuse
4- trophoblast proliferation: diffuse, severe
-----------------------------------------------------------------------------------------
* The chromosomes in complete mole are paternal ( androgenesis); the fertilized ovum either contains no chromosomes or inactivated chromosomes.
** Theca lutein cysts are produced by incrased HCG, and may be found also with placental hypertrophy of Rh- isoimmunization, or multiple pregnancy, or even with normal singleton pregnancy. The cysts are variable in size, from few millimeters up to 10 cm.
--------------------------------------------------------------------------------------------
Incidence:
- Geography: occurs 1: 1000 in most of the world including the USA. Much increased in certain parts of Asia.
- Age incidence: increased incidence in pregnancies towards the extremes of childbearing period ( <20>40 years).
- Recurrence : 1-2 % of cases of previous moles.
Clinical Features:
Symptoms appear later in the 1st trimester or during 2nd trimester and are more severe with complete mole. These include:
1. Bleeding per vagina: it is the most common symptom. It is of variable amounts. It may be described as 'prune juice ' appearance.
2. Uterine size: large for dates in 50% of cases of complete moles with doughy sensation. May be small for date in partial moles and some cases of complete moles. It may coincide with date in come cases.
3- Fetal activity: FHS not detected although the uterus is above symphysis.
4- Preeclampsia : because Preeclampsia is rarely seen before 24 weeks, if present before that time it suggests molar pregnancy .
5- Hyperemesis gravidarum.
5. Embolisation with trophoblastic tissue with or without villi.
6. Thyrotoxicosis: plasma T4 is elevated may be due to thyrotropin-like action of HCG , or variants TSH produced by molar tissue.
7. Spontaneous expulsion of grape-like vesicles per vagina.
Diagnosis:
Diagnosis is made by the following:
1- Clinical features (vide supra)
2- Ultrasound: very useful in the diagnosis;
(a). Complete mole: picture 'snow storm' or 'honeycomb appearance' with no fetal parts.
(b). Partial mole: picture of missed abortion.
3- Serum β-HCG levels are much higher than expected for the gestational age.
Prognosis:
Maternal mortality: currently mortality from molar pregnancy is reduced to ZERO by more prompt diagnosis and appropriate therapy.
Morbidity:
1. Anemia from bleeding
2. Intrauterine infection and sepsis.
3. Malignant transformation (choriocarcinoma); complete mole (20%), partial mole (4-8%)
Treatment
Treatment of vesicular mole consists of 2 phases;
[A]. Immediate evacuation of molar tissue, and
[B]. Subsequent follow-up for detection of persistent trophoblastic proliferation or malignant transformation.
I. Pre-treatment evaluation:
1. CBC and hemoglobin or hematocrit estimation.
2. Blood transfusion prepared.
3. Searching for metastasis; chest X-ray, if positive(i.e. cannon ball sign), CT chest, liver, brain is indicated.
4. Serum β-HCG estimation to be used as a baseline level for follow-up
5. Medical fitness, and pre-operative assessment .
II. Termination of pregnancy (Evacuation of the mole)
[A]. Vacuum Aspiration; method of choice for evacuation of the hydatidiform mole whatever the uterine size. For large moles, a wide caliber IV line should be established and blood should be ready for transfusion if needed. After complete evacuation of molar tissue, gentle uterine curettage is done. Biopsy from the uterine contents & curettage is sent for histopathology. The procedure may be done under ultrasound guidance. The procedure may be complicated by severe uterine bleeding or uterine perforation.
[B]. Surgical evacuation; using ring forceps and curettage. It is inferior to suction, and may be used in small sized uterus in absence of suction apparatus.
[C]. Oxytocin, Prostaglandins, and Hysterotomy; are no longer used in the management of molar pregnancy.
[D]. Hysterectomy; may be rarely done in certain circumstances;
1. Perforation of the uterus with internal hemorrhage.
2. Age above 40 with sufficient number of children.
III. Prophylactic Chemotherapy:
§ Its role in improving the long term prognosis lacks the evidence.
§ The toxicity from it may be significant including death.
IV. Follow up Procedure:
The prime objective is to early detect malignant changes.
A general method of follow up is as follows;
Contraception for at least ONE year best by COCs (as they suppress LH that cross- react with HCG).
Serum βHCG measurement every 2 weeks.
Once the level is normal (i.e. lower limit of measure for the laboratory) then test βHCG monthly for 6months, then every 2 months for a total of 1 year. Follow up is discontinued and pregnancy allowed after one year.
A rise or persistent plateau in the level requires evaluation & usually therapy.
The following lines of treatment are deferred in the management of molar pregnancy:
Medical evacuation.
Hysterotomy.
Prophylactic chemotherapy
Thursday, January 3, 2008
SOME STATISTICAL HINTS
Some Statistical Hints;
-Sensitivity= the ability of the test to diagnose the disease in its presence: i.e. = true positive / all positive by the reference test (TP+FN)
-Specificity= the ability of the test to exclude the disease in its absence. i.e = true negative/ all negative by the reference test(TN+FP)
-Positive predictive value= [TP/ all positive by the screening test(TP+FP) ]x 100
-Negative predictive value = [TN/all negative by the screening test( TN+FN)]X100
-DIAGNOSTIC ACCURACY = [(TP+TN)/all studied (TP+FP+TN+FN)]X 100
-True positive (TP)= positive by screeninig test and by reference test
-True negative (TN)= negative by screeninig test and by reference testfalsepositive (FP)= positive by screening test BUT negative by reference test
-False negative (FN)= negativeby screening test BUT positive by reference test

